
IMRT stands for Intensity Modulated Radiotherapy. It the most refined form of radiotherapy planning. Cancers have irregular shapes. IMRT provides us an ability to exactly localize our treatment to the shape of the target. Even concave shapes can be defined using IMRT which are not possible using even 3D-conformal radiotherapy. All this could be achieved by using advanced computer systems and better imaging facilities like CT and MRI. The planner in IMRT gives constraints the normal tissues, depending on there tolerance levels. Then using sophisticated algorithms plans are generated. Also in 3D conformal radiotherapy a constant dose is given through a field, while in IMRT plans the intensity of the dose given can be modulated by movement of the multileaf collimators. Studies have shown significantly lesser rectal and bladder toxicities using IMRT plans compared to 3D conformal plans.
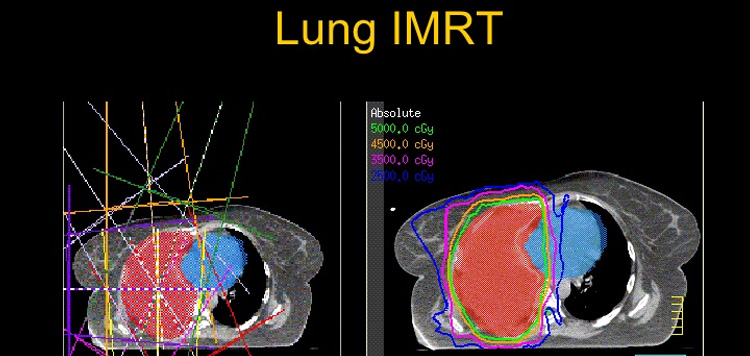
Intensity-modulated radiation therapy (IMRT) is an advanced mode of high-precision radiotherapy that uses computer-controlled linear accelerators to deliver precise radiation doses to a malignant tumor or specific areas within the tumor. IMRT allows for the radiation dose to conform more precisely to the three-dimensional (3-D) shape of the tumor by modulating—or controlling—the intensity of the radiation beam in multiple small volumes. IMRT also allows higher radiation doses to be focused to regions within the tumor while minimizing the dose to surrounding normal critical structures. Treatment is carefully planned by using 3-D computed tomography (CT) or magnetic resonance (MRI) images of the patient in conjunction with computerized dose calculations to determine the dose intensity pattern that will best conform to the tumor shape. Typically, combinations of multiple intensity-modulated fields coming from different beam directions produce a custom tailored radiation dose that maximizes tumor dose while also minimizing the dose to adjacent normal tissues.
Because the ratio of normal tissue dose to tumor dose is reduced to a minimum with the IMRT approach, higher and more effective radiation doses can safely be delivered to tumors with fewer side effects compared with conventional radiotherapy techniques. IMRT also has the potential to reduce treatment toxicity, even when doses are not increased. Due to its complexity, IMRT does require slightly longer daily treatment times and additional planning and safety checks before the patient can start the treatment than conventional radiotherapy.
Currently, IMRT is being used most extensively to treat cancers of the prostate, head and neck, and central nervous system. IMRT has also been used in limited situations to treat breast, thyroid, lung, as well as in gastrointestinal, gynecologic malignancies and certain types of sarcomas. IMRT may also be beneficial for treating pediatric malignancies.
Radiation therapy, including IMRT, stops cancer cells from dividing and growing, thus slowing or stopping tumor growth. In many cases, radiation therapy is capable of killing all of the cancer cells, thus shrinking or eliminating tumors.
Most facilities rely on a specially trained team for IMRT delivery. This team includes the radiation oncologist, medical physicist, dosimetrist, radiation therapist and radiation therapy nurse.
The radiation oncologist, a specially trained physician, first consults with the patient to determine whether radiation therapy with IMRT is the most appropriate treatment. After obtaining informed consent, the individualized course of treatment is planned. A radiation physicist, who has specialized training in the field of radiation oncology physics, ensures the linear accelerator delivers the precise radiation dose and that computerized dose calculations are accurate. A dosimetrist works with the medical physicist to calculate the IMRT exposures and beam configurations necessary to deliver the dose prescribed by the radiation oncologist. The final treatment plan is verified on the machine with measurement by the medical physicist before being delivered to the patient. A highly trained radiation therapist positions the patient on the treatment table and operates the machine. The radiation oncology nurse assesses the patient and provides the patient with additional information about the treatment and possible adverse reactions. The radiation oncology nurse also helps in managing any reactions or side effects from treatment that may occur, in collaboration with the physician.
A medical linear accelerator (LINAC) generates the photons, or x-rays, used in IMRT. The machine is the size of a small car—approximately 10 feet high and 15 feet long. The energy of the photon or x-ray, in the order of 10 millions of volts, is generated by the LINAC to penetrate the patient's body to the tumor. During the 15 or so minutes of treatment, the patient is required to lie still on the treatment couch while the linear accelerator delivers multiple beams of radiation to the tumor from various directions. The intensity of each beam's radiation dose is dynamically varied according to treatment plan. The patient usually will not feel any sensation while the radiation is on, but will hear noise from the machine, and may smell an odor from the electronic equipment, or see the warning indicator light. The noises and odors from the machine are normal. The patient will be in the room alone during the treatment period with constant monitoring from the radiation therapists from outside the treatment room.
The radiation therapist operates the equipment from a radiation-protected area nearby. The therapist is able to communicate with the patient throughout the procedure. The therapist observes the patient on closed circuit television.
IMRT often requires multiple or fractionated treatment sessions. Several factors come into play when determining the total number of IMRT sessions and radiation dose. The oncologist considers the type, location and size of the malignant tumor, doses to critical normal structures, as well as the patient's health. Typically, patients are scheduled for IMRT sessions five days a week for five to eight weeks.
At the beginning of the treatment session, the therapist positions the patient on the treatment table, guided by the marks on the skin defining the treatment area. If molded devices were made, they will be used to help the patient maintain the proper position. The patient may be repositioned during the procedure. Imaging systems on the treatment machine such as x-ray or CT may be used to check positioning and marker location. Treatment sessions usually take between 10 and 30 minutes.